Just for fun, print and try this quiz!
When your wife has stage 4 metastatic breast cancer, and has been hospitalized once for an upper extremity DVT, once for pneumonia, another time for malignant pleural and pericardial effusions, has had small pulmonary emboli, and then gets diagnosed with leptomenigeal carcinomatosis, and you also live in a world that has Google, so you can type in those terms (or worse click on the links some idiot put in a blog post) and get very detailed descriptions of these diagnoses and, more importantly, their prognoses, then, despite the doctors not coming right out and telling you so, you kinda have to face it that the most likely hand you’ll get dealt this year is to watch her die. Not just the mostly likely hand, but the most likely 99 hands.
We’ve tried from the start (of the stage 4 diagnosis), before the more in-your-face evidence (which for me was the hospitalizations) not to live in denial, and not to keep things from our two teenagers or our family or community. To make decisions taking this possibility/probability into real account. But this turns out to be much more difficult that I expected.
 So this post is about a concept called Death Straight Talk (let’s call it DST. That way it sounds like the more familiar “DNR”). There are three arenas in which I want to talk about DST: 1) the medical world, doctors, nurses, and Medicine as an institution; 2) family, friends and community; and 3) the metaphysics of probability and how we think about our future. So here we go.
So this post is about a concept called Death Straight Talk (let’s call it DST. That way it sounds like the more familiar “DNR”). There are three arenas in which I want to talk about DST: 1) the medical world, doctors, nurses, and Medicine as an institution; 2) family, friends and community; and 3) the metaphysics of probability and how we think about our future. So here we go.
1) DST in Medicine: Hospice operates on an agreed-upon basis of DST. The idea is that “there’s nothing left to do” to prolong life (meaningfully), so shift the medical care to comfort, pain control, and getting the most of out each day. A Do Not Resuscitate (DNR) order is another form of DST in medicine, where the patient gets to issue a token that goes in their chart saying something like, “Look, I’ve thought this through and I’ve come to the conclusion that death is preferable to life after resuscitation, so let me go.” These are both DST items that have been embodied in institutional practice, the first at a more macro level, because, it turns out, Hospice care ties in deeply to the structure of how and what things get paid for and who gets to decide. (This in itself is worth a whole other post, but life’s too short for me to dig into that.) The second is at the more micro level, because it’s just about what to do under certain circumstances for an individual patient, whether in hospice or not.
These two patterns, Hospice and DNR, are formal recognition that near death, things are different, and we have to act differently. But now to my direct experience: despite an ominous prognosis, Ellen’s not at either of those two points yet, and so, institutionally, there’s practically no DST. It’s like a binary switch: either we act like you won’t die, and plan our doctoring on that, or we finally give up and off you go to Hospice. Here’s how this plays out. Hospitals are places full of protocols: vitals every 2 or 4 hours, neurological checks every hour, gotta pee before you get discharged, NPO (nil per os – no food or drink) before surgery, start a bag of fluids for practically anything, keep for observation for two days after X surgery, don’t go off the floor (or out of the ward doors), and on and on. Lots of protocols, mostly in place for good reasons.
But here’s the question: if you might have only 4-6 weeks left of life (if the current spread of cancer doesn’t respond to therapy) do those protocols apply? Should you really spend those two days under observation, living a substantial percentage of your remaining life in the hospital instead of at home? Should you really have that conversation you’re having with your family or friends interrupted so the nurse can write down your blood pressure numbers? Should you really have to spend the more than an hour a day (once you add it up) explaining your complex medical history over and over to each new nurse, resident, attending, etc., who comes to check up on you? Should you really get filled with IV fluids before a surgery to offset the dehydration risk that comes from the NPO protocol, which is there to mitigate the risk of throwing up under anesthesia, when those same fluids have a high risk – shown in the previous hospitalization – of causing swelling in your legs and feet which might make it painful to impossible to walk in your last weeks of life?
In our experience the protocols just don’t take into account DST. Here’s how I know: during our last hospital visit, I explicitly told nurses and doctors a story that approximately went like this: “Please treat us as if Ellen’s chart had a big DST sticker in it. It’s kind of like DNR but stands for Death Straight Talk [I really said that], which, like a DNR, is treatment instructions for you from Ellen, but what it means is: first of all, we can, and do, talk about death straight, but second and more importantly, in providing your care, think about whether your actions are appropriate for someone who will likely die soon.”
The results of telling this story were clear: after some initial shocked looks, we got different care. The doctors let us go home “early” after Ellen’s Ommaya reservoir implant; we got “off-floor-privileges” while awaiting surgery; they didn’t make Ellen start on fluids at midnight before the surgery, etc. The humans involved responded deeply and with compassion to the truth that was embodied in a simple acronym: DST.
2) DST with family, friends, and community: If you want to create drama, lie. Lie explicitly, unconsciously, or by omission. In our case, we might call that Death Curvy Talk, or Death Denial Talk (DDT). The other night Ellen and I watched a dumb movie called “Meet My Valentine,” which is about a guy diagnosed with terminal brain cancer who decides not to tell his family but instead find a replacement husband/father for them instead. As a movie it was really dumb because that DDT was so obviously poisonous. But as a metaphor it’s revealing. If I look at where things feel twisty and drama-filled and out of whack, I see that I haven’t lived up to DST. As I said at the beginning of this post, we’ve tried to face things directly from the start. But something interesting has happened since the introduction of the DST acronym. As a token that we can refer to, it’s given us permission, or an opening, or something to actually get to to the straight talk more quickly. Now that it’s there, we invoke it. “Hey, I have a DST thing…”
Here’s a quote from an e-mail from a friend: “I wanted to offer to help, if need be, to begin/continue/whatever, discussion of burial, funeral directors etc. I have, unfortunately, intimate experience with this recently, as you know, and might be able to bring some perspective to this part of DST.” What a relief and and efficiency that this provides. It feels to me that the more I live into DST, the more this experience goes from what I call “dramatic” to what feels “powerful” or “moving.”
3) DST metaphysics and probability: Here’s the problem with DST. It assumes we know the specific future. Of course in one sense we do. All of us will die, we know that, but that’s hardly a specific knowing. So, using DST, how do we also talk straight about that one other hand of cards out of the 100–the one in which it turns out that Ellen recovers and later quietly dies in her sleep at the ripe old age of 103 well after I’m gone? This is the hard part for me. I used the metaphor that Ellen’s disease prognosis is like drawing a hand of cards. But that’s, at the very best, only a partially valid metaphor. Probability provides a great tool set for assessing aggregate outcomes, but it also can have the effect of deep dis-empowerment at the individual level. Just because your chances of getting breast cancer go up by X% if you have the BRCA1 mutation doesn’t mean that you don’t have any agency in whether it actually happens in your own body. From all our reading, it’s pretty clear to us that cancer as a bodily process is connected to the immune system, which is deeply connected to the central nervous system, and also connected to physiological terrain. So what power does that mean we actually have? I believe that diet, and stress, and my thoughts have an effect on “my chances” of getting cancer, and these are things I have control over. Bookstores, however, are filled with conclusions from this that to me are just magical thinking: that you can just think yourself back to health. But I also read and hear people jump to “don’t blame the victim” as soon as you mention the ways in which we do have agency. It’s kind of a double bind: if you believe in agency, then if you got sick or don’t heal yourself it’s your fault. But if you just take it as luck of the draw (i.e., not your fault) then how can you activate where you do have agency?
So to me this is where I don’t know how to have real DST. What is the “straight talk” that both acknowledges and deepens the agency we do have, and yet doesn’t fall prey to either magical thinking or blame-the-victim? Just because the odds are 99 to 1, does that mean we have to match the relative percentages of our talking time to those odds?
I don’t know the answers to these questions. But the core move in DST gives me guidance: open myself to what exists, or at least turn towards it rather than away.
Modern disease prognoses provide odds based on existing historical records: scientific studies. Open myself to them. But also the evidence of agency affecting cancer outcomes exists. Open myself to it. My pain and my joy in these days exists. Open myself to both of them. Paradoxically, denial and hiding and self-veiling also exist. So that’s OK, too; turning-toward will also periodically involve turning-away. This isn’t about some moral claim. It’s just a wish, a longing, perhaps a stance, to turn towards what I see in front of me. DST. Last words: just because I don’t wish to turn away from that which I do see, that doesn’t preclude me from turning toward that which I don’t see: all the potential branches of the future. Because what else is creation?
–Eric Harris-Braun
Thanks to good drugs, I had no nausea or vomiting after my double chemo last Thursday. Go, Emend! I don’t care how expensive you are–I love you. I do seem to be more worn out than usual. Or than I expected. Since my legs felt stronger, I went for a walk beyond the mailboxes on Thursday or Friday, and I made it back! With a few rests. But this weekend I have mostly sat around and indulged in Netflix, at least when not learning new blog posting technologies such as below.
In general, though, I feel all right and I’m doing pretty well at taking care of myself except for the things that require two functioning hands. Unfortunately, this includes putting on most shirts and other important self-care tasks. My hands are damaged from chemo-induced neuropathy and we don’t know yet whether, now that I’m on a different chemo regimen or two, they will get worse or better. My feet are still pretty bad, especially the left one, which feels like a block of tingly wood that does not want to be touched. That left foot is the major cause of my unsteadiness walking.
Here is last week’s community Shaker Lemon Pie story out loud:



In England in late September my left arm started to swell up a bit–mostly it seemed like my hand. This is the arm with the DVT (blood clot) under the collarbone, and thus the arm I’ve been wearing a lymphedema compression sleeve on since early April to try to prevent lymphedema from developing. Lymphedema is common in an arm when you’ve had lymph nodes in your armpit removed as part of breast cancer surgery, which I have–in 2006–though I never had a bit of trouble or swelling with it before the DVT. Anyway the DVT is a risk factor for lymphedema too, because it causes venous congestion, which is a different kind of swelling but can interfere with lymph drainage. You have a whole set of lymph vessels and lymph nodes in your body that collect and drain lymph fluid as part of your immune system–lymph takes away the used-up after-effects of infection and your body’s fight against infection. Lymph nodes are the stations along the way where your body kills off organisms that shouldn’t be in your system (making more by-products to get rid of). Then it all drains into your bloodstream at the end. So it’s kind of like the Gowanus Canal–you don’t want it to just SIT there not moving.
You can check out this image to show the lymphatic system: Diagram of lymphatic system if you’re interested
Anyway there I was with possible lymphedema, but before I knew it I had blood clots in my lungs, and wasn’t allowed to follow up on the arm swelling because massaging the arm/shoulder might loosen up a few more clots. So I didn’t get to go until I was safely back on blood thinners for a while–Thursday before last. I learned how to wrap my arm in “graduated compression” bandages and look like a mummy. This, along with gentle massage of the lymph channels from my hand to my neck including my left side, would encourage the static lymph fluid to move along as it should. But it might take many weeks. ARGH! Another self-care thing to do, and this one takes about 20 minutes a day. Just what I needed. Then before my next followup appointment I was in the hospital with pneumonia. So I had to cancel last week’s appointments but it was really working! So I was excited to go in on Tuesday and show off my progress. Which was indeed impressive. (I think it’s because it was only a month of not treating it–not enough time for the lymph vessels themselves to get too damaged, so the flow out of my arm can still happen the regular way rather than slowly through the tissue itself. (Remember, everything in the circulatory system and lymph system works by differential pressures of different substances, and everything moves toward a lower-pressure area if it can. Veins and lymph vessels don’t pump their fluids themselves at all.)
Anyway, for some geeky reason I thought it would be fun to show how the graduated-compression wrapping works. So here is a brief photo series.
The prescription is to wrap the arm 23 hours a day!
When it’s time to redo the compression wrapping, first I take all the wrappings off my arm.
Then I shower. Then I apply more moisturizer than I normally would.
Then I tackle rolling up the bandages again (which are like Ace bandages but you don’t stretch them much at all).

So here are all the things I need, all ready for the wrap job. (Which I have decided to consider as a craft project.)
3 bandages in different widths, but first: the stockingette sleeve and the foam layer.
Then three bandages, finally secured with those little clips.
It all takes about 10 minutes from here.
First the stockingette sleeve with a hole cut for the thumb. This protects the arm skin.
Then the foam strip gets wrapped from the thumb around the arm up to the upper arm and tucked in to itself. This provides more padding and protection for the arm.
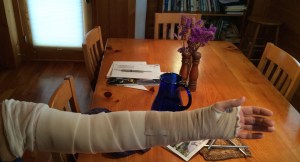
Next comes the narrow bandage that starts at the wrist and wraps over the hand 3-4 times, then goes up the arm until the end. Then a piece of surgical tape secures it (though again, it isn’t wrapped very tightly).
Don’t tape the foam or it rips!
Next the medium-width bandage, which starts below the wrist and goes up as high as it goes, then gets taped.
You’re supposed to avoid wrinkles in the bandages. But you also wrap it loosely enough that you can move your elbow freely.
Finally I put on the third, widest bandage, which often needs some assistance to get right, because though it starts below the elbow, it goes almost to the shoulder and it’s hard to do it right way up there where I can’t really see.
That bandage gets secured with the clips and then–pro tip!–tape goes over the clips to keep their sharp edges from catching on my clothes.
Then the extra stockingette gets pulled down over the top of the bandage to further protect my tender skin.
Voila! All done until the next shower.
And it’s working really well! They told me 4-6 weeks of wrapping before the arm would go down enough to stop wrapping and switch to a new fit and strength of compression sleeve instea, but by next week I’ll be ready for that step. Yay! (You should have seen the left arm–on the right in this picture–a couple weeks ago. It looked like a quite overweight person’s arm–still arm-shaped, but really big and round in all dimensions, and tense.
 What a relief that something is going right! Even better than expected.
What a relief that something is going right! Even better than expected.
I need that right now because I’m still knocked out by the pneumonia (and blood clots in the lungs) and everything else seems like a big challenge everywhere I turn.
We are receiving so much help and company that it is easy to keep my mood basically positive most of the time, though.
My liver enzymes went back to normal yesterday so I got chemo–we’re calling it day 1 of cycle 22 with a skipped dose on day 8 of cycle 21. Last week was my unplanned week off of chemo–last Tuesday my enzymes were still too high for the oncologist to be comfortable, so no chemo, and instead, a visit to the liver specialist upstairs at Albany Med later in the week.
That was a reassuring consult, because my enzyme elevations were called “mild” in the liver-disease context, and the blood testing has ruled out any disease causing the elevations (hepatitis, etc.). The fellow working with the specialist told me liver metastases don’t raise the enzyme counts (confirming something I had already heard from someone else but wasn’t sure about). And the specialist ended up talking to my oncologist and reassuring him that I could still get chemo with mild enzyme elevations if the chemo was of benefit–it was unlikely to damage my liver. So! All that is good. Even though we still don’t know what caused the late-April ALT/AST elevations–if not Sudafed plus everything else. They even tested my Epstein-Barr Virus titer and it didn’t show anything active. The liver specialist thinks it could have been the chemo drug itself, since that happened to 18% of takers in one trial, but on the other hand, I’m on month 16 of the same drug and it hasn’t had that effect on me. So. Water under the bridge–I hope so. And if that same water cycles by again, we can desist from freaking about about it so much. Thank you, liver specialist!
I suggested my oncologist take a deep breath and let the liver thing go now, but he said “I don’t take deep breaths. I’m just going to worry about next week’s enzyme levels.” Well, I’m not (much).
Meanwhile I have sent in my paperwork for disability (and eventual Medicare if I want). That was a lot of work. Since the DVT I have felt honestly more disabled by my situation, though it’s often disability-via-too-many-appointments rather than disability-via-physical-inability. Though I’ve got some of that too. I am trying to return to two walks a day, but they are shorter and leave me tired. I’m also trying to stick to doing my 30-minute PT routine once a day, and ideally do some qi gong once a day as well. That’s a lot! (I do it with the help of my neighbors here at QIVC, who join in with me and encourage me and provide interesting conversation.) And that routine is not something I’m holding myself to on days like today, post-chemo, post-bone-medicine-that-causes-flu-like-symptoms, and post-IV-vitamin-C treatment (feels like ick also). I took the 2 shorter walks but I don’t think PT or qi gong is going to happen: I am tucked in bed with my head feeling like bleh.
Despite feeling icky today I was lucky enough to enjoy a delicious lunch at my friend Gina’s house…so lucky to have a friend who loves to cook and share! I cannot describe how good that quiche or related eggy thing tasted…ahhhh.
So, curb cuts. Here is how I’m living a slightly different version of life now. When crossing the street in Chatham or Albany, I go for the curb cuts. It now apparently matters, to an unconscious part of me that directs my feet, whether I have to pick up my leading foot that extra 4″ or so, or whether there is a nice slope for that interim step between street and sidewalk. Conserve energy! I guess that’s what I am doing. I just noticed this a week or so ago.
Next week ideally will be chemo again on Tuesday, then various brain-zap set-up appointments Wednesday and Thursday. Same for Tuesday the next week, then zapping on Wednesday the 27th. So that’s the plan! More later on the metastasis spreadsheet, which I actually pulled off, and shared with my oncologist and radiation oncologist. Next: conquer the world with it (the world of radiology at least).
I greatly enjoyed perusing this illustration from a Scientific American article (thanks, Paul): “How Oncolytic Viruses Destroy Tumors”
Ahhhhh wouldn’t that be great?
Thinking about my various lab results (bloodwork done every chemo day), I was wondering if there were patterns between Week 1 and Week 2 that I wasn’t seeing, or patterns that would explain the bouncing of my red blood cell count. It didn’t seem predictable at all, though I would have predicted something like: best on Week 1 (after 2 weeks without chemo) and worse on Week 2 (only 1 week after a dose of chemo). But then blood cells have their own life cycle. So I wanted to see if anything made sense. AND our mathematician friends were visiting. The result: some amusing geeking out in Excel and then Google Charts at the dining table, and this:
WBC=white blood cell count, RBC=red blood cell count, HGB=hemoglobin, AST & ALT are liver enzymes. Values for Week 1 and Week 2 of the chemo cycle are shown in matching pairs of colors–bright and lighter. (Values were normalized so they would all show nicely on the same graph.) Pretty, huh? Next it would be fun to graph them all in relation to their normal values, somehow.
So this is the kind of thing I try to eat for lunch and dinner these days: spinach salad, black bean soup, sauteed squash, sauteed mushrooms, and roasted new potatoes with homemade ají (Ecuador-style hot sauce). Glass of water not pictured. Of course I did snack on some whole-wheat crackers earlier in the day…
Tomorrow I start a new chemo cycle (I believe it’s cycle 13).
People have been asking: “How many rounds of chemo do you have to do?” or “When will you be done with chemo?” There is no solid answer to that question because we don’t know what is going to happen. But here is my understanding of how it sometimes goes:
So my answer to “When will you be done with chemo?” is sometimes “Never, I hope!” Because if something’s working, without bad side effects, why would I stop?
I think in cases where people’s cancer just goes away, and they are “NED” (no evidence of disease), they sometimes stop chemo. Also, people take breaks from chemo (for holidays, or trips, or just to recover from side effects).
But there are also people who ditch standard medical treatment–often when it stops working well for them–and try alternative or complementary treatments or integrative treatment strategies (standard plus complementary treatments). Which I have been looking into, for sure, because standard chemotherapy in the end doesn’t have that much to offer.