Link Best bald-head covering advice I’ve encountered
Much has been going on in the last week, which I will write about soon, but in the meantime here is a source of info for anyone else has had to give up their hair to chemotherapy. I am expecting this might be me in 2 to 3 weeks.
It even taught me a few new tricks!
The only thing she left out was the need to pad your bald head to make hats fit or to make a thin head covering look like there is hair underneath it.
Start of Phase Two

 I am at NY Oncology Hematology getting my first dose of my first cycle of my second chemotherapy regimen: Gemzar (gemcitabine) and carboplatin. I like to sit in an out-of-the-way corner because it’s quieter–no chair neighbors watching TV. It’s the same chemo schedule as before–Day 1 and Day 8 of a 21-day cycle–but very different drugs with more recognizable “chemo sucks” side effects.
I am at NY Oncology Hematology getting my first dose of my first cycle of my second chemotherapy regimen: Gemzar (gemcitabine) and carboplatin. I like to sit in an out-of-the-way corner because it’s quieter–no chair neighbors watching TV. It’s the same chemo schedule as before–Day 1 and Day 8 of a 21-day cycle–but very different drugs with more recognizable “chemo sucks” side effects.
I have been very lucky to be on a chemo drug without those side effects all these months! (22 months to be exact).
But now my cancer has begun, as my oncologist said Wednesday, “to start acting the way we expect of triple-negative breast cancer.” Meaning the Eribulin stopped preventing new sites of disease from developing, and up they popped. Last week’s CT scans showed all this:
—the many small “spots” in my lungs grew, showing that they are metastases (which we pretty much knew)
—there’s a 1 cm lesion in my pancreas and some mysterious associated fluid collection around the pancreas
—another small tumor seems to have developed on one adrenal gland
–there are two enlarged lymph nodes in my abdomen
—in the lining behind my left lung was about a liter of fluid that was a mix of blood and pleural fluid. Not sure what caused that, exactly, but it is likely due to some more tiny cancer cells blocking the normal drainage of the area between the two pleural layers (some fluid is normal). I had it drained by the pulmonologist on Wednesday–they took out 600 ml and said there was more in other smaller “pockets” they didn’t bother to drain. Now we have to wait and see whether the fluid will collect again.
Other than the pleural effusion compressing my left lung and adding to my shortness of breath, none of these new things cause any symptoms. We hope that the two new chemo drugs will control or reduce them as well as keep control of my two original mets (R lung and sternum).
So I had a full month off of chemo. And now it’s back to the negotiating tables since the cancer decided it had a lot more things to say to me.
Improving the blog!
My friend Lisa is helping me to set up e-mail notifications so that when I add a blog entry, anyone who likes can get notified of it by e-mail. It’s not quite working yet but…close! Stand by for future exciting technological announcements.
Vanities: usefulness
(Part three of four musings on vanity’s role in my life.) I have always enjoyed being a person who is useful, who gets things done, who follows through on details, who is handy, who helps others more than needs help herself. I can still be that person in some realms, but not others. I am riding out some big changes in what I do with my life energy and trying not to let them get me down or make me feel less of a valuable person than before.
But. I am a Certified Professional Midwife but no longer attend births. That is big. I gave up being the primary midwife for homebirth clients just a few months after my diagnosis; I had one pregnant client when I was diagnosed and was committed to seeing that through, but I could tell I would not have the space in my new life to keep that up. I assisted at a few births here and there after that, but the last one was in January. Now I am not healthy enough to get up and go to a birth in the middle of the night. And whether I would have the energy and focus to be someone’s midwife, even for a prenatal visit, is not predictable from day to day. But it’s not just on that level that I can’t practice midwifery right now; being someone’s midwife means taking responsibility for someone’s care and prioritizing their needs sometimes over one’s own. Being seriously ill means I can’t hold that space for someone else; to do it with full intent and generosity requires emotional and practical and what I think I have to call spiritual dedication that I just can’t afford.
So I am no longer serving women and families in the way I planned to do.
For the last 10 years I have worked with Eric as project manager of our shared Web projects and also as a junior programmer (learning as I went along from him). But the stretches of time when I feel able to dig in and write code, or debug code, are pretty few these days. When I had chemo in 2006, it took me 8 months afterwards before my brain was clear enough to really start programming again. So maybe some of the same thing is going on, or maybe it just takes a level of focus that is hard to attain in between appointments, taking medication, various self-care tasks, and feeling too bad sometimes to concentrate on anything much. So in the realm of programming I am not useful right now (even for my favorite project, the MANA Stats Project).
I’m unsteady on the stairs so I can’t carry a laundry basket up or down, and right now I’m too weak and out of breath to carry our big salad bowl to potluck. I am no longer the person who carries a visitor’s suitcase up the stairs. In fact, I seldom carry my own backpack.
I am always looking out for things I can still do, like empty the dish rack or dishwasher, pay the bills, make calls, deal with the junk mail, and fold the laundry (while seated on the couch). I like to find favors to do for people with the skills and abilities and time that I have–like fix an earring, or superglue a mug back together, or do the paperwork to sign a friend up for EZ-Pass. It’s important to me to still be useful–somehow. I am vain about, or overly attached to, being that person in the lives of others. When I can’t be useful, and the flow of help is even more one-way than it is now, will I still be as accepted and as loved?
P.S. Friends say that having the opportunity to help me and love me is the favor I am doing them, the gift I am giving them now. I hear that, but I think I am maybe not big-hearted enough to really understand it yet.
“Chemo holiday”?
I’m currently on a bit of a ‘chemo holiday” to see if that helps with my various pain symptoms and the neuropathy. I got numb fingers two weeks ago, which led to me calling off the Eribulin last week and the oncologist’s suggestion of a “holiday” to give my body some off time and see if the chemo is contributing to or causing the various pains I have (mostly back and knee). So this is my usual week off, but i skipped my second dose of chemo from cycle 30 last week. II have CT scans next week, and then the week after we meet with the oncologist again to see what to do. (That’s a l-o-n-g scan interv-hell!)
If the cancer hasn’t grown then probably a cycle’s worth of holiday (3 weeks) before beginning another chemo—one that doesn’t have a big risk of neuropathy. If it has grown then no more holiday, I’ll start on something. Maybe Xeloda, which is suspected to maybe get into the brain (good for me). We decided not to dig into that decision until we need to. The chemo drugs known to work best for triple-negative breast cancer (TNBC) also have a high risk of neuropathy, so for now they are not options. Newer drugs (that may actually work just as well for me) have less risk.
The next step should be entering a clinical trial of a PARP inhibitor, very likely to work well on me because I have TNBC, but I need to be off steroids to be eligible. And I am far from being off steroids, unfortunately. But tapering down slowly–I have made it from 50 to 27 mg of Prednisone since the beginning of September. Headaches continue, but not any worse. And I have a new medicine to try that is aimed at headache reduction, starting tonight.
We’ll see what happens with my “lung spots”—I am hoping they are just sitting there still being mysterious and tiny.
Vanities: function
Moving on to the next kind of vanity (part two of four)…
Vanity about function: My body doesn’t do what it used to do. One year ago, I jogged three miles with my sister and probably went for a walk later on in the day, too. Back then I was doing interval training most days as well as walking two miles and often jogging a mile or so. I felt great. But it’s been a tough year, this Year Two of stage IV cancer. I am lucky to get a Year Two, I know, but it has been hard on me for sure.
I used to have good balance; now because of my numb left foot and my leg weakness, I am unsteady. When I stand still, I wobble. When I do qi gong, I lose my balance and have to grab for a chair or wall. When I start to move, sometimes I kind of lurch on my left foot. When I am walking, I feel better if I have three points of contact instead of just two. That means I run my hand along railings or just touch a wall, or hold Eric’s hand or arm. If my hands are full and I’m going upstairs, I run my elbow against the wall. I don’t need to hold on, but I need to have something to lean against if I lurch or lose my balance. And of course coming downstairs, I think about falling; I watch my step carefully and I hold on to the railing and I can’t have both hands full.
The numb foot also means I’m at risk of falling down: if that foot encounters something unexpected, like a tilt in the pavement or an apple in the dark on the farm road, it twists outward and doesn’t alert me soon enough for me to correct the imbalance. And my legs are sometimes too weak to catch myself, too. So I fall over to the left. Only about once every week or two! Sustaining no damage–it’s an easy fall.
I noticed this in July in France: I used to be the person who got out of the way by stepping off the curb, nimbly, when I and an oncoming walker had to negotiate a narrow sidewalk. Now I’m the person who sticks to the sidewalk and I make the other person give way, because I need to keep up my steady path on even footing.
Right now I can’t go for a real walk. For a long time my legs have felt weak, like I just finished a 10-mile hike, but I could ignore that–they didn’t feel worse with exercise–until recently, when I think they really did get weaker due to inactivity during the pneumonia. Right now a “short walk” means walking to the mailboxes and back. A long walk is if I get out on the road, which I only have managed once in the last week or two. My knee keeps me not walking, too, but I’ve been able to ignore that in the past. So it feels like it’s the lungs and legs that are keeping me from walking, or, in my case, strolling.
It’s a bit of effort now to stand up, or lean over and straighten up again, and I use my arms to help get out of chairs. Sometimes I think I shouldn’t do that, because it will just allow my legs to stay weak. But sometimes I’m just too tired to challenge myself. Every time I stand up I give myself a couple of seconds to get grounded and make sure I’m not dizzy. Also I plot my progress through the hazards of living room furniture or the mess on Jesse’s floor, because I might trip or bang into something.

Since my hospital stay, we have been driving up the farm road to the house about half the time–the half when I feel more tired and will wear myself out walking from the parking area by the road. This is so ironic because I have been the person most defensive of the no-cars-on-the-farm-road practice the community agreed to. I was the one who was so happy when we agreed to put a sawhorse at the start of the farm road to cue people that they should park, not drive right up to the house (including driving on the lawn because what, no driveway?). And now who’s moving that sawhorse to the side on a regular basis? Why, us. It’s like a little ironic knife-twist in my side every time we do it.
It is hard to accept that right now I am so wobbly and weak and out of breath, and harder to contemplate that this might not be so temporary–that “recovery” in this context might restore some of my function but won’t bring me back to a year ago.
All of this means I now can’t hide in the world of the well. Even in that world, I show up as a sick person, whether I want to or not. And of course I don’t want to! The other day, a week after I got home from the hospital, I walked into a local farm & produce store. The walk from the car to inside the store was about 20 feet. I went in the double doors and paused on the floor mat, to plan my next direction so as not to wander and waste my energy. The woman behind the counter saw this and asked me if I was okay. I said I was. Then she offered to get me a chair to sit on. I explained I’d had pneumonia and I was just taking it slow. She went and got me a chair anyway, and showed it to me later when I passed by the counter. So, you know, my cover was blown the moment I walked in and paused! I bet I looked pale and wobbly too.
Fatigue means I ask for people to do stuff for me a lot–as much as my ego can handle–like go upstairs for something, or get me something to drink, or carry my backpack for me on the way to the car. Eric and I have a well-balanced dance of asking/not asking/assuming/not assuming that most often works really well–he doesn’t assume I need help with everything, and when he offers help he’s very matter-of-fact rather than anxious or over-solicitous. Sometimes I ask him to start something (like a dish for dinner) but I want to finish it because I want to have done something, and that’s okay too.
But really, it’s shocking to me how different my capabilities are from a year ago. How diminished. Am I this person? I did not sign up for this.
Vanities: appearance
I’ve been thinking about vanity a lot lately. I seem to have a lot of it. To me it settles out into some different realms:
Vanity about body appearance: from taking steroids for so long, I have chubby cheeks and a more rectangular face without noticeable cheekbones. My face really looks different from before. I was kind of dreading the steroid face all along, and here it is. No pictures of me look nice to me. It took me a month or so to stop not-recognizing my face in the mirror. This chubby-face thing really bums me out. I liked my old face and this is yet another sign of the mandatory ongoing negotiations with cancer.



I’ve also gained weight elsewhere on the steroids–that and a lack of ability to exercise much lately–and steroid weight goes to the midsection so I’ve got more of a belly than usual and my pants are tight around the waist. I was really feeling good about myself when I weighed 142 pounds and exercised every day; now I weigh 152 pounds instead and feel like there’s little I can do about it.
The combination of steroids and edema from my left arm means I have a double chin and maybe even a triple chin if I try, on the left side anyway. Who said that was allowed?
My hair is really thin; in August and September about half of it fell out slowly, and I don’t know why. Chemo? Steroids (possible)? Anyway I now have curly, more-gray-than-before, sparse hair. My scalp shines through. On first glance it might not look weird but I am definitely sporting the “chemo victim” look all the time now, like it or not. The curls that want to go straight up are not really what I wished for all those times I wished for curly instead of stick-straight hair.
On the other hand, this summer sometime my eyebrows grew back. For a while I had basically half an eyebrow on one side and 2/3 an eyebrow on the other side, and I had an eyebrow pencil and eyebrow mascara to make them look normal. Now I don’t need to bother, so that’s nice!
But the way I look now overall gives the game away: I am an ill person, not a healthy person. I am far more self-conscious now when I go places, like the chiropractor or even my oncologist’s offfice. In the waiting room, I’m one of the obviously in-treatment And when I dig into how I feel about this transformation, I find a lot of vanity about my previous appearance–which I was very happy with–and grief that I have lost that, and with it my own feeling of being attractive. I really liked my cheekbones.
Status Two years?
Yesterday was the two-year anniversary of when I found out I had stage IV cancer.
Gallery Welcome to lymphedema!
In England in late September my left arm started to swell up a bit–mostly it seemed like my hand. This is the arm with the DVT (blood clot) under the collarbone, and thus the arm I’ve been wearing a lymphedema compression sleeve on since early April to try to prevent lymphedema from developing. Lymphedema is common in an arm when you’ve had lymph nodes in your armpit removed as part of breast cancer surgery, which I have–in 2006–though I never had a bit of trouble or swelling with it before the DVT. Anyway the DVT is a risk factor for lymphedema too, because it causes venous congestion, which is a different kind of swelling but can interfere with lymph drainage. You have a whole set of lymph vessels and lymph nodes in your body that collect and drain lymph fluid as part of your immune system–lymph takes away the used-up after-effects of infection and your body’s fight against infection. Lymph nodes are the stations along the way where your body kills off organisms that shouldn’t be in your system (making more by-products to get rid of). Then it all drains into your bloodstream at the end. So it’s kind of like the Gowanus Canal–you don’t want it to just SIT there not moving.
You can check out this image to show the lymphatic system: Diagram of lymphatic system if you’re interested
Anyway there I was with possible lymphedema, but before I knew it I had blood clots in my lungs, and wasn’t allowed to follow up on the arm swelling because massaging the arm/shoulder might loosen up a few more clots. So I didn’t get to go until I was safely back on blood thinners for a while–Thursday before last. I learned how to wrap my arm in “graduated compression” bandages and look like a mummy. This, along with gentle massage of the lymph channels from my hand to my neck including my left side, would encourage the static lymph fluid to move along as it should. But it might take many weeks. ARGH! Another self-care thing to do, and this one takes about 20 minutes a day. Just what I needed. Then before my next followup appointment I was in the hospital with pneumonia. So I had to cancel last week’s appointments but it was really working! So I was excited to go in on Tuesday and show off my progress. Which was indeed impressive. (I think it’s because it was only a month of not treating it–not enough time for the lymph vessels themselves to get too damaged, so the flow out of my arm can still happen the regular way rather than slowly through the tissue itself. (Remember, everything in the circulatory system and lymph system works by differential pressures of different substances, and everything moves toward a lower-pressure area if it can. Veins and lymph vessels don’t pump their fluids themselves at all.)
Anyway, for some geeky reason I thought it would be fun to show how the graduated-compression wrapping works. So here is a brief photo series.
The prescription is to wrap the arm 23 hours a day!
When it’s time to redo the compression wrapping, first I take all the wrappings off my arm.
Then I shower. Then I apply more moisturizer than I normally would.
Then I tackle rolling up the bandages again (which are like Ace bandages but you don’t stretch them much at all).

So here are all the things I need, all ready for the wrap job. (Which I have decided to consider as a craft project.)
3 bandages in different widths, but first: the stockingette sleeve and the foam layer.
Then three bandages, finally secured with those little clips.
It all takes about 10 minutes from here.
First the stockingette sleeve with a hole cut for the thumb. This protects the arm skin.
Then the foam strip gets wrapped from the thumb around the arm up to the upper arm and tucked in to itself. This provides more padding and protection for the arm.
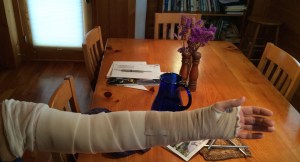
Next comes the narrow bandage that starts at the wrist and wraps over the hand 3-4 times, then goes up the arm until the end. Then a piece of surgical tape secures it (though again, it isn’t wrapped very tightly).
Don’t tape the foam or it rips!
Next the medium-width bandage, which starts below the wrist and goes up as high as it goes, then gets taped.
You’re supposed to avoid wrinkles in the bandages. But you also wrap it loosely enough that you can move your elbow freely.
Finally I put on the third, widest bandage, which often needs some assistance to get right, because though it starts below the elbow, it goes almost to the shoulder and it’s hard to do it right way up there where I can’t really see.
That bandage gets secured with the clips and then–pro tip!–tape goes over the clips to keep their sharp edges from catching on my clothes.
Then the extra stockingette gets pulled down over the top of the bandage to further protect my tender skin.
Voila! All done until the next shower.
And it’s working really well! They told me 4-6 weeks of wrapping before the arm would go down enough to stop wrapping and switch to a new fit and strength of compression sleeve instea, but by next week I’ll be ready for that step. Yay! (You should have seen the left arm–on the right in this picture–a couple weeks ago. It looked like a quite overweight person’s arm–still arm-shaped, but really big and round in all dimensions, and tense.
 What a relief that something is going right! Even better than expected.
What a relief that something is going right! Even better than expected.
I need that right now because I’m still knocked out by the pneumonia (and blood clots in the lungs) and everything else seems like a big challenge everywhere I turn.
We are receiving so much help and company that it is easy to keep my mood basically positive most of the time, though.
Quick update
It’s Sunday afternoon and guess what? I still have pneumonia. (I have to keep reminding myself of this to explain why I am still so, so, so very tired and worn out.) We came home late Thursday afternoon and I keep waiting to notice I’m feeling better, but I don’t notice. I am doing much less coughing, though.
I didn’t have a headache at all on Wednesday or Thursday in the hospital, but we can’t figure out why. Oxygen? Antibiotics? Now that I’m home the headache is back, which is really getting me down.
Anyway, the plan for the next week is: rest as much as possible, take antibiotics, and eventually feel better. Then the week after that, back to chemo. I guess I’m just skipping the second dose of round 29.




