Friday 12/18 after chemo I was feeling pretty good overall–the Zofran was working to keep nausea away and I didn’t feel too bad. But then Saturday I woke up feeling totally knocked down. I couldn’t walk to the bathroom without help. Not only were my major muscles weak, I felt sort of like sludge was in my blood vessels instead of blood. Sunday afternoon we talked to my oncologist and decided to go to he ER to find out what was going on–most likely the pleural effusion had built up again and would need a more aggressive solution than the one-time drainage of the previous Wednesday.
In the ER they use an ultrasound to confirm that the pleural effusion was back and was interfering with my breathing and oxygenation. But as an early Christmas present, they also followed some clues from the EKG they did to find out that I had fluid around my heart as well. That was not an emergency, but needed to be dealt with pretty soon before it became dangerous. So I was admitted to Albany Medical Center yet again to have two procedures done the next day: a drainage catheter put in to the space around my heart for a couple of days and a more permanent catheter installed to drain the space around the left lung.

I spent Sunday night in the hospital, had the two procedures both done on Monday afternoon, and was discharged on Thursday, Christmas Eve. Since then I have been home sitting on the couch or in the bed waiting to feel better and having Eric drain fluid out of my lung every afternoon. How romantic!
We went to NYOH yesterday to see about chemo, which was on the schedule, but I didn’t really feel well enough yet. My feet and legs are really swollen from the IV fluids I got in the hospital and it’s painful to walk. I guess I am less out of breath now. So that’s the short story of the latest bumps in the road. There may be more to do with the heart, depending on whether the fluid is building up again. Both buildups are caused by tiny cancer cells blocking the drainage of normal fluid, so killing the cells off is really the only solid solution.
In other news, both kids are home from school and my mom is visiting so there are lots of people around to help this invalid get through the day.
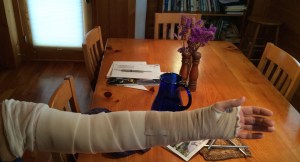
In other bad news, the reason I need so much help is that the neuropathy in my hands got worse enough during my time in the hospital that I can’t touch-type anymore, and can’t do a lot of other things, like buttons and opening jars, requiring reasonably working hands. Besides them being clumsy and numb, one hand also hurts when touched by almost anything, or used, or lowered below the waist.

In the plus column I’ve gotten the lymphedema in my left arm under control so I can wear the lighter and more comfortable compression sleeve and gauntlet during the day and only wrap my arm in the graduated-compression bandages at night. In the hospital, though, it was bandages 24/7 and the nursing staff put up a sign–which seemed so obvious given the big bulky bandages that we felt compelled to add to it:
“No BP Left Arm”
“(No SpO2, no IV, no lifejacket storage)”